Introduction to periodontal ligament
The periodontal ligament (PDL) is derived from the dental sac tissue, which invests the tooth germ. It is a complex, vascular, and highly cellular soft connective tissue interposed between roots of the teeth and the inner wall of the alveolar socket. It has the shape of an “hour glass” and is narrowest at the midroot level. The PDL consists of a fibrous stroma in a gel of ground substance containing cells, blood vessels and nerves 202. Many terms have been used previously to describe periodontal ligament, including desmondont, gomphosis, peri-cementum, dental periosteum, alveolodental ligament, and periodontal membrane. It has a rapid turnover rate and high remodeling capacity because of which it has the ability to adapt and maintain a constant width despite being exposed to rapidly changing physical forces such as mastication, speech and orthodontic tooth movement 203, 204. Also, PDL has a remarkable capacity for renewal and repair, playing a pivotal role in periodontal regeneration. Major functions of PDL are formative, nutritive, proprioceptive, supportive and homeostasis. Let us now discuss various aspects of PDL in detail.
Development of periodontal ligament
At the onset of PDL formation, the PDL space is filled with unrecognized connective tissue. The first step in the formation of PDL is the formation of fringe fibers, which are newly synthesized nascent fiber bundles. These fibers are formed on the newly formed root dentine and along the bone surfaces and are deposited by elongated, highly polarized fibroblasts. These fibers are tightly packed with the deposition of acellular extrinsic fiber cementum by cementoblasts. As the tooth erupts, these fringe fibers merge across the width of the periodontal ligament and make the principal fiber bundles of PDL. These fiber bundles become embedded on one side in cementum and on the other side in alveolar bone and are referred to as Sharpey’s fibers. The orientation of these fibers changes with the eruption of the tooth. Initially, before tooth eruption the CEJ is below the alveolar crest. So, the PDL fibers are oriented obliquely. As the tooth erupts, the CEJ coincides with alveolar crest. So, just below the free gingival fibers oblique fibers become horizontally aligned (alveolar crest fibers). The middle zone of the PDL is formed of collagen fiber splicing and unsplicing designed to accommodate minor tooth movements. This area is referred to as intermediate plexus.
Along with the PDL fibers which make up to 70% of the total volume of PDL, the remaining 30% is occupied by the dense connective tissue, which is composed of blood vessels, lymphatic vessels, and nerve fibers (Table). The inflammatory cells can be seen in the perivascular spaces, the number of which increases during inflammation. Garant (2003) 205 has subdivided periodontal ligament into three regions,
- A bone-related region, rich in cells and blood vessels.
- A cementum-related region, characterized by dense, well-ordered collagen bundles.
- A middle zone containing fewer cells and thinner collagen fibrils.
Components of PDL
Structurally, human PDL consists of collagen fibers (53-57%), blood vessels and nerve endings (1-2%) that are embedded in an amorphous mucopolysaccharide matrix 207.
Periodontal ligament fibers
The fibers in PDL tissue mainly comprise of collagen and elastic fibers. The principal fibers of the PDL are primarily composed of collagen Type I and Type III. Collagen Type III is known as fetal collagen and is important in the early phases of wound healing. Other collagens such as Types VI and XII are also present in PDL, but in lesser quantity 208, 209. The principal Fibers have distinct collagen fiber bundles with their terminal ends inserting into the cementum and alveolar bone (Sharpey’s fibers). The principal fibers inserted into the bone are widely separated as compared to those inserted into cementum. Also, these fibers are fewer in number as compared to those entering the cementum 210-212. The diameter of these fiber bundles varies from 1-4 μm. Three-dimensionally, the path of these fibers from the cementum to the bone is not just radial but may also be tangential. Furthermore, these fibers may cross each other, thus providing reinforcement to one another.

The Sharpey’s fibers present on the distal root surfaces are longer with distinct appositional lines in the alveolar bone as compared to the mesial surface of the root. This is because the teeth move in a mesial direction throughout life. So, there is continued deposition of bone opposite to the distal root surface as compared to the mesial root surface where it is resorbed and deposited in alternate cycles. It creates scalloped “reversal lines” in the alveolar bone
Along with the principal fibers which run from the cementum to the bone, there are also fibers which run parallel to the root surface, designated as “indifferent fiber plexus” 213, 214. These fibers are primarily seen in the apical half of the root. These fibers may also get incorporated into the mineralized matrix of bone or cementum, like the Sharpey’s fibers. According to Sloan and Carter 215, the PDL fibers are arranged in following distinct groups of principal fibers,
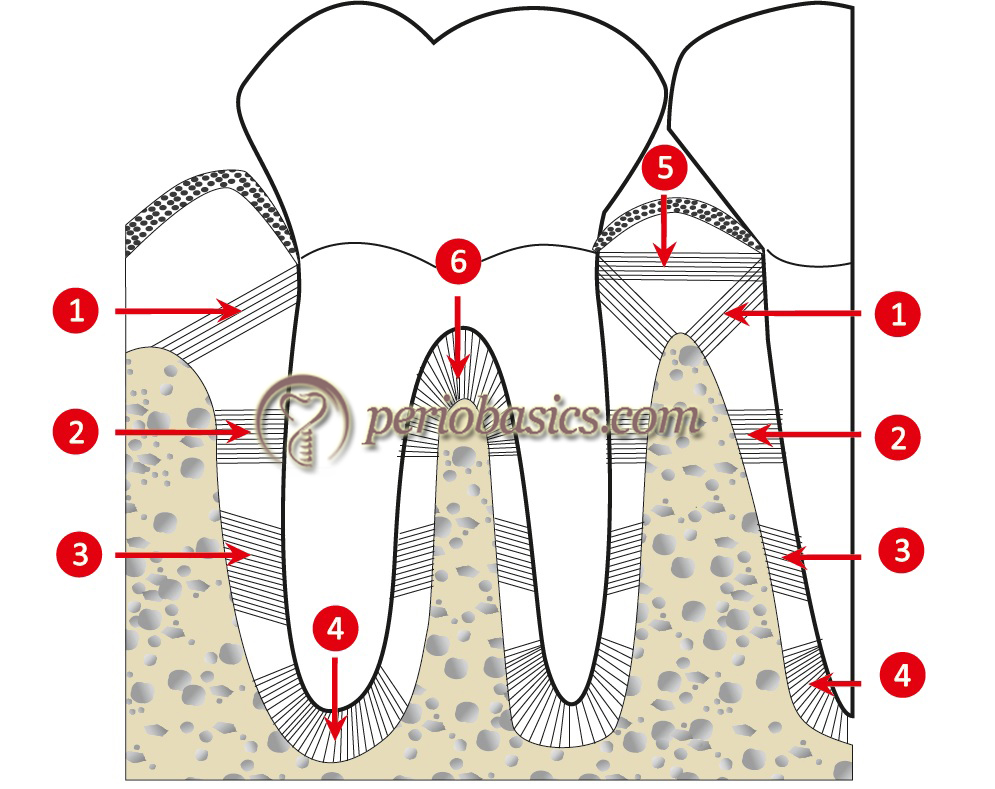
Dentogingival fibers:
These fibers run outwards from the tooth surface into the gingival connective tissue.
Alveolar crest group:
These fibers are inserted into the cementum and alveolar crest apical to the junctional epithelium. They function to retain the tooth in the socket by countering the coronal thrust. These fibers also resist the lateral movement of the tooth.
Horizontal group:
These fibers insert at right angles into the cementum and alveolar bone. Their function is same as that of the alveolar crest group.
Oblique group:
These form the largest group of fibers occupying…………………. Content available in the hard copy of the website……….. Content available in the hard copy of the website……….. Content available in the hard copy of the website
Periobasics A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Cellular components of periodontal ligament
There is a variety of cells present in PDL involved in the maintenance of its normal structural organization, including fibroblasts, undifferentiated mesenchymal cells, epithelial cell rests of Malassez, osteoblasts, cementoblasts, osteoclasts, odontoclasts and defense cells. These cells are involved in constant remodeling of the PDL, cementum, and alveolar bone.
Fibroblasts:
Principal cells involved in PDL homeostasis and regeneration are fibroblasts 225. Unlike the gingival fibroblasts which are derived from the general mesenchyme, the PDL fibroblasts are ecto-mesenchymal in origin 226. Structurally, the fibroblasts are spindle-shaped with an elongated appearance in vitro 227. In vivo, fibroblasts demonstrate an irregular disc-shape with a mean diameter of about 30 μm 228. These cells demonstrate all the features of an actively synthesizing cell such as abundant rough endoplasmic reticulum, mitochondria, Golgi complex, and vesicles. In PDL, the fibroblasts are oriented parallel to the ligament fiber bundles and they wrap around them with their cytoplasmic processes 229. When stained with colloidal silver, they demonstrate either one or two regions of acidic proteins which are associated with nucleolar organizer regions. The PDL fibroblasts contain lysosomes, which are large membrane-bound vesicles containing a homogenous matrix that is more electron-dense than the surrounding cytoplasm.
Differences between periodontal and gingival fibroblasts
| Periodontal ligament fibroblasts | Gingival fibroblasts |
|---|---|
| PDL fibroblasts are derived from the dental follicle (sac), a derivative of the neural crest ectomesenchyme. | Gingival fibroblasts are derived from perifollicular mesenchyme, a derivative of the stomodeal mesoderm. |
| PDL fibroblasts get juxtaposed to the tooth surface soon after the disruption of the root sheath. | During development of the periodontium, gingival fibroblasts do not come into contact with the tooth surface. |
| PDL fibroblasts are primarily of two types. Majority of them have regular connective tissue fibroblasts like characteristics. A subpopulation of PDL fibroblasts has osteoblasts like characteristics. | There is only single type of gingival fibroblasts. |
| Most fibroblasts in the PDL contain large amounts of rough endoplasmic reticulum and well-developed Golgi complexes, indicative of a high rate of protein synthesis. | Gingival fibroblasts show considerable variation in their morphological development ranging from highly synthesizing fibroblasts to fibroblasts that show signs of swelling and degeneration. These changes are probably the result of site to site variation in cytokines and other inflammatory mediators. |
| .............. Content available in the book............. | .............. Content available in the book............. |
| .............. Content available in the book............. | .............. Content available in the book............. |
| .............. Content available in the book............. | .............. Content available in the book............. |
| .............. Content available in the book............. | .............. Content available in the book............. |
The PDL fibroblasts have some unique properties such as, they exhibit osteoblastic properties like alkaline phosphatase activity 230, responsiveness to parathyroid hormone 231 and the production of bone sialoprotein in response to 1,25-dihydroxyvitamin D 231. Also, these cells have been shown to 3 possess proteins related to the osteoblastic activity, including, osteocalcin 232, osteopontin 233, periostin 234, osteonectin, runt related transcription factor-2 (RUNX-2) and osterix 235. It has been shown that the PDL fibroblasts possess receptor activator of NF-kappa B ligand (RANKL) and osteoprotegerin (OPG). Both RANKL and OPG play a key role in the bone metabolism 236. They also express desmoplakins which have been considered to protect gap junctions in these cells against cell transformation caused by cell contraction during orthodontic tooth movement and periodontal repair 237. The PDL fibroblasts may look alike microscopically, but they have been shown to have different sub-populations. Whether or not these subpopulations have been derived from a single progenitor cell is still not clear.
These cells also have immunological properties. It has been demonstrated that PDL fibroblasts have functional characteristics of leukocytes and leukocyte-derived cells, functioning in innate immune response 238. Furthermore, it has been demonstrated that on stimulation with bacterial lipopolysaccharides, PDL fibroblasts up-regulate transcription of various cytokines and chemokines 238.
Know More…
Is periodontal ligament collagen degradation extracellular or intracellular:
The degradation of the PDL collagen fibers was historically considered as an extracellular process which involved collagenases. In extracellular collagen degradation, collagenases are responsible for cleaving the triple-helical portion of the molecules within the fibrils into 1/4-3/4 fragments with further degradation of these molecules by gelatinases. Before initiation of the collagenase activity, the surface glycoproteins are removed by stromelysins. Although collagen degradation is an extracellular process, in PDL the collagen degradation is primarily an intracellular process. It has also been suggested that the intracellular collagen degradation is not unique to PDL but is found in all healthy tissues where there is controlled turnover and remodeling 239. Only in pathological tissue changes and/or when degradation is rapid and involves the whole tissue simultaneously, does the extracellular path-ways have a role.
Undifferentiated mesenchymal stem cells
These cells are predominant in the central portion of the ligament, in close proximity to the blood vessels 240. These cells remain within the PDL throughout life and are responsible for tissue homeostasis 241. These cells help in maintaining the normal PDL space as they have the ability to differentiate into the formative as well as resorptive cells.
Know More…
Periodontal ligament stem cells and periodontal regeneration:
A stem cell is the one which has the capability of self-renewal and differentiation into various cell lineages. Originally, the human mesenchymal stem cells (MSCs) were isolated from aspirates of adult bone marrow 242. Presently, stem cells have been isolated from various tissues like bone marrow, adipose tissue, placenta and muscle 243, 244. Because PDL is ectomesodermal in origin, it also harbors a small population of stem cells derived from dental follicle. These cells are believed to have the capability to differentiate into fibroblasts, osteoblasts, and cementoblasts. All these cells are required for periodontal regeneration. Seo et al. 245 in 2004 initially isolated multi-potent PDL stem cell population from the extracted third molar. These cells have been shown to express …………. Content available in the hard copy of the website………….. Content available in the hard copy of the website……… Content available in the hard copy of the website….
Epithelial cell rests
The epithelial cell rests of Malassez were first described by Malassez in 1885 from the sections of human teeth. These cells are commonly seen close to the cementum with their distribution varying according to the stage of tooth eruption and the age of the subject 252-259. The exact function of these cells is unclear, but they could be involved in the periodontal repair/regeneration. These cells may also have an important role in the maintenance of PDL and differentiation of cementoblasts 260. Because these cells are never in contact with the bone and a thin buffer zone of fibrous connective tissue separates them from the bone, they may possibly act as ankylosis inhibitors 261. With age, the cellularity of these cells decreases 262. The epithelial cell rests show rapid proliferation when cultured in vitro. So, these cells have been implicated in the development of periodontal cysts 261, 263 and formation of periodontal pocket 257. The epithelial cell rests also express ameloblastin which is a non-amelogenin enamel matrix protein that plays an important role in the differentiation of ameloblasts and induction of cementoblasts in association with amelogenin 264. However, the exact function of ameloblastin in these cells is not clear 265.
Know More…
Role of epithelial cell rests of Malassez in periodontal regeneration:
Regeneration of the lost periodontal tissue due to periodontal diseases is the ultimate goal of periodontal treatment. Regeneration involves the formation of new cementum, new bone and attachment of new PDL fibers to newly formed cementum and bone 266-268. Many cells are involved in periodontal regeneration including the PDL fibroblasts, gingival connective tissue fibroblasts, cementoblasts, osteoblasts, endothelial cells and macrophages 269. A lot of investigations have been done on various periodontal tissues to evaluate their capability to regenerate the lost periodontal structure and architecture. But, the most commonly overlooked cells in periodontal regeneration which are present within the periodontal ligament are the ………. Content available in the hard copy of the website……… Content available in the hard copy of the website……… Content available in the hard copy of the website…………
Osteoblasts
Osteoblasts within the PDL are found on the surface of the alveolar bone. Their appearance and structure is similar to the osteoblasts found in any other part of the body. Active osteoblasts have strongly basic cytoplasm with a prominent nucleus which lies towards the basal end of the cell and a pale juxtanuclear area indicates the site of the Golgi complex. An active osteoblast demonstrates all the features of actively synthesizing cells, such as prominent rough endoplasmic reticulum and numerous mitochondria. Active osteoblasts make a layer of cuboidal-shaped cells on the surface of the bone and are connected to each other via gap junctions and also via simplified desmosomes. They also contact to the osteocytes lying within lacunae in the adjacent bone via gap junctions, thus creating a well-organized system through the bone tissue.
The precursor cells for the osteoblasts are seen adjacent to the layer of active osteoblast in the vicinity of adjacent blood capillaries. These cells possess a reduced cytoplasm and few organelles. They differentiate to form mature osteoblasts. These cells migrate to the ………….. Content available in the hard copy of the website……… Content available in the hard copy of the website……… Content available in the hard copy of the website……………… Content available in the hard copy of the website……… Content available in the hard copy of the website……… Content available in the hard copy of the website…………
Periobasics A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Osteoclasts
These are the bone resorption cells, which play a key role in bone remodeling. These are large multinucleated cells found within the resorption lacunae of the bone. They have a ruffled border adjacent to the resorbing surface, enclosed by a smooth ‘clear’ zone. They have numerous mitochondria near the ruffled border, suggesting their high metabolic activity. These cells resorb the bone in two stages. Initially, there is the demineralization of minerals from the bone margin and then exposed organic matrix is degraded. In inactive osteoclasts, the ruffled border is absent. The multinucleated cells which are associated with the cementum and dentine resorption are referred to as cementoclasts and odontoclasts, respectively.
Defense cells
The PDL contains defense cells, including macrophages, mast cells, and eosinophils. These cells are involved in the generation of the immune response during periodontal inflammation. These cells have been described in detail earlier in ‘cellular components of gingival connective tissue’.
Ground substance
The ground substance of PDL is made up of high water content of up to 70%. It is primarily composed of two main components which are glycosaminoglycans/proteoglycans and glycoproteins. The ground substance of PDL is composed of various glycosaminoglycans such as hyaluronic acid, heparan sulfate, dermatan sulfate, chondroitin sulfate and proteoglycans of which dermatan sulfate is the principal one. Major glycoproteins present in the PDL ground substance are fibronectin and laminin. These are discussed in detail as follows,
Glycosaminoglycans and Proteoglycans in PDL ground substance
Glycosaminoglycans and proteoglycans are the primary components of the ground substance of PDL connective tissue.
Glycosaminoglycans
Glycosaminoglycans are long chains of repeated disaccharide units comprising of hexosamine and uronic acid. These molecules act as a binding material and due to their hydrophilic nature, they hold large amounts of water 279. Following are the major glycosaminoglycans in PDL ground substance,
Hyaluronic acid:
This is a high molecular weight glycosaminoglycan having widespread distribution in the connective tissue, especially in embryonic tissues and cartilage. It can bind to CD44 molecules through which it adheres to other matrix components. The primary function of this molecule is hydration of the ground substance, mediating interactions between cells and matrix and supporting vascular development.
Chondroitin sulfate:
It is a proteoglycan composed of disaccharide units of “O” sulfated N-acetyl galactosamine and D-glucuronic acid. Depending on the site of sulphation, the molecule is termed as chondroitin-4-sulfate or chondroitin-6-sulfate. It functions as a solvent in the extracellular matrix and binds various connective tissue elements.
Dermatan sulfate:
This molecule is similar to chondroitin sulfate except that glucuronic acid is exchanged by L-iduronic acid. These molecules engage the collagen fibers in the connective tissue and are especially predominant in the epithelial-connective tissue interface.
Proteoglycans
As already discussed in ‘ground substance of gingiva’, structurally proteoglycans have a core protein bound to one or more glycosaminoglycan chains. Various proteoglycans found in PDL ground substance are decorin, biglycan, versican, fibromodulin, lumican, periostin and Cd44 280, 281.
Decorin:
The name decorin is based on the ability of this proteoglycan to bind to collagen that can be seen with an electron microscope as “decorations” on the collagen fibrils 282, 283. This proteoglycan was formerly known as ……………….. Content available in the hard copy of the website……… Content available in the hard copy of the website……… Content available in the hard copy of the website…………
Periobasics A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Biglycan:
Biglycan is a dermatan/ chondroitin sulfate proteoglycan which was formerly known as PG-I 287. It is widely distributed in the connective tissue including articular cartilages, intervertebral discs, skin, tendons, bones, and gingiva. It is found in association with the cell surface and pericellular matrix 288. Biglycan appears to play an important role in the mineralization process, although the precise nature of its role is still to be determined. Decorin and biglycan appear to have antagonistic roles in mineralization process. Decorin appears to have an inhibitory role during mineralization 289 whereas biglycan is one of the mineralization nucleator 290. Biglycan has also been suspected to be a receptor of amelogenin expression and enamel formation 291.
Versican:
It is a chondroitin sulfate proteoglycan primarily found in loose connective tissue. It is a large molecule thought to be secreted by fibroblasts 284. The core protein of the molecules consists of an epidermal growth factor-like and lectin-like amino acid sequences, whereas the amino acid terminal has a hyaluronic acid-binding region. There are 14 glycosaminoglycan attachment sites in the core protein. Versican plays an important role in facilitating the binding of cell surface glycoproteins to the extracellular matrix 292. It has also been reported to play a role in fibroblast migration 293.
Fibromodulin and lumican:
These proteoglycans are rich in keratin sulfate and bind to collagen fibers present in the PDL. It has got structural similarities with both decorin and biglycan. Because it binds to the collagen fibers, it may modulate the collagen fiber formation. Studies using knockout mouse models have suggested that fibromodulin and lumican are involved in the supramolecular organization of PDL collagen 294.
Periostin:
This proteoglycan has been recently found in PDL ground substance. It has been so named because it was initially found in the periosteum. This molecule has a disulfide-linked protein that favors osteoblast attachment and spreading. Periostin is highly expressed in molar and incisor PDL 295. It can interact with collagen Type I 296 and has been proposed to play a role in the response of PDL to mechanical stress because it has been found to be present more in pressure than in areas of tension. It has been demonstrated that periostin dimers crosslink the collagen matrix 297. Furthermore, it has been demonstrated that in periostin-mutant mice, incisor-eruption is defective and is characterized by a disorganized PDL 295. Hence, it can be concluded that due to the ability of periostin to bind to collagen Type I, it plays an important role in the maintenance of PDL.
CD44:
The CD44 was formerly known as lymphocyte homing receptor or Hermes antigen 298-300. It is a transmembrane glycoprotein with its cytoplasmic domain associated with actin microfilaments. It can bind fibronectin, laminin, and collagen and it may also be a receptor for hyaluronan 301.
Glycoproteins
These are protein molecules, covalently bound to carbohydrates. They have a widespread distribution in the connective tissue. Their main function is of binding the cells to the extracellular matrix elements. Major glycoproteins found in PDL ground substance are fibronectin, laminin, nidogen, vitronectin, tenascin and thrombospondin. Fibronectin and laminin have already been discussed in the section on ‘macromolecular components of gingival connective tissue’.
Nidogen:
Nidogens are ubiquitous basement membrane glycoproteins. They are also known as Entactins. There are two types of entactins expressed in vertebrates named entactin-1 (~150 kDa) and entactin-2 (~200 kDa) (or nidogen-1 and nidogen-2). These molecules bind non-covalently to the laminin and acts as a bridge between laminin and collagen Type IV. The nidogen-laminin complex is essential for the integrity of the basement membrane.
Vitronectin:
Vitronectin is a 75-kDa glycoprotein which has a widespread distribution in the mesenchymal tissues. The major function of this molecule is to bind various connective tissue elements. It interacts with the extracellular matrix through its collagen and heparin binding domains, and with cells through its RGD integrin-binding sequence. Another important function of vitronectin is that it is conducive to osteoblast differentiation.
Tenascin:
This glycoprotein is a large molecule with star-shaped structure. The tenascin glycoprotein family includes tenascin-C, tenascin-R, tenascin-W, tenascin-X, and tenascin-Y. They bind to fibronectin and to proteoglycans, particularly the cell surface proteoglycan, syndecan. In PDL, tenascin-C has been shown to have a localized distribution toward the attachment zone to the bone 302.
Thrombospondin:
These are a family of structurally related multi-functional, multimodular, calcium-binding extracellular matrix glycoproteins encoded by separate genes. There are five members in thrombospondin family which have been divided into two groups where thrombospondin-1 and -2 belong to group-A and thrombospondin-3,-4 and -5 belong to group-B. Thrombospondins have binding properties and it binds to various extracellular matrix components such as integrins, fibronectin, collagen, and laminin. Also, thrombospondins bind to various cells and platelets.
Normal periodontal ligament Space
The average width of human PDL space is 250 μm or 0.25 mm with a range from 0.15 to 0.38 mm 303. In rats, it is around 150 μm 304, in monkeys around 250 μm 305, in pigs around 250 μm, and in bovine around 500 μm 306. Radiographically, it can be seen as a thin radiolucent line covering the tooth root. The width of PDL varies according to the functional state of the tooth. Teeth with trauma from occlusion characteristically show widening of PDL space.
Vascular supply of periodontal ligament
The main blood supply of PDL in the maxillary and the mandibular arches is by superior and inferior alveolar arteries, respectively. The PDL is particularly rich in its blood supply because it not only has high metabolism but also has peculiar mechanical and functional demands. When occlusal forces are subjected on the PDL, they are not only absorbed by the ligament fibers, but also by means of tissue fluid transfer within the PDL space, also referred to as ‘hydraulic pressure distribution’. The most important vessels in maxilla providing arterial supply to the PDL are anterior and posterior superior alveolar arteries, infraorbital artery, and the palatine artery. In the mandible, these arteries are the mandibular artery, sublingual artery, the mental artery and buccal and the facial artery. Around the PDL, there are primarily three sources of blood vessels. These are, Apical group of arteries: These are branches of vessels supplying the tooth pulp.
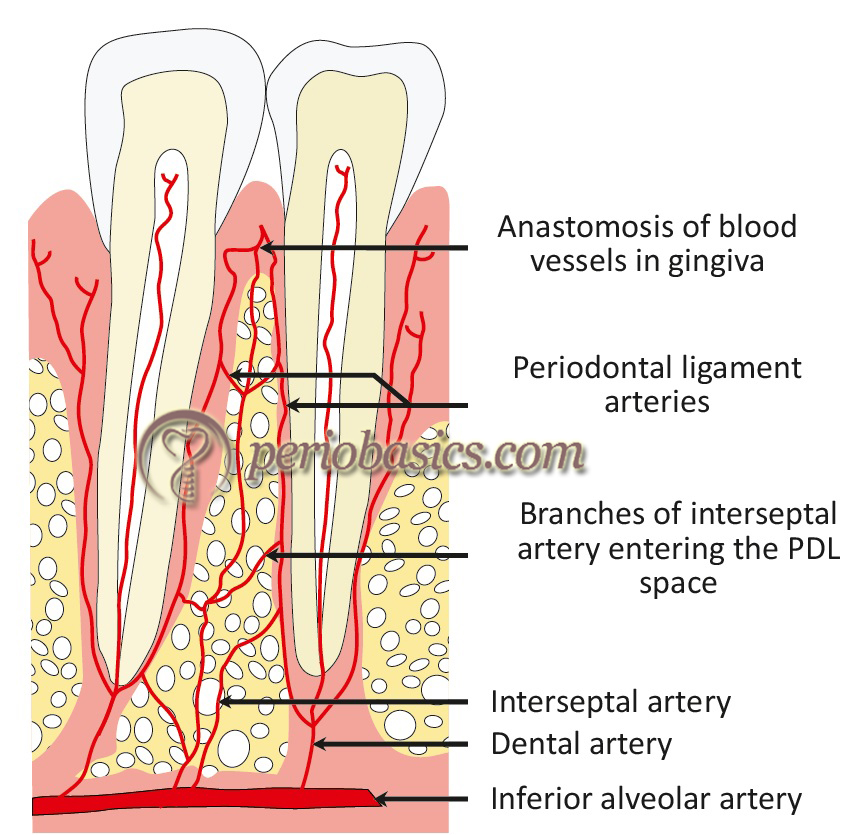
Alveolar group of arteries:
These arteries enter the PDL space from the alveolar bone. These are also referred to as perforating arteries. They arborize in the coronal and apical direction.
Gingival group of arteries:
These are derived from the gingival blood supply. These enter the PDL from the crestal region and anastomoses with the vascular network of PDL. The venous and lymphatic vessels are located close to the blood vessels. The veins from the PDL drain either into the interdental veins or into the periapical plexus. The lymphatic vessels drain into the regional lymph nodes, finally draining into the thoracic duct.
Innervation of the periodontium
PDL has both sensory and autonomic nerve supply. The sensory supply of PDL of maxillary and mandibular teeth is by the trigeminal nerve. In the maxilla, it is by the second branch and in the mandible, it is by the third branch of the trigeminal nerve. The sensory myelinated nerves enter the PDL at apical foramen region and run coronally, gradually losing their myelin sheath 307-309. Other nerve endings enter the PDL through alveolar bone and branch occluso-apically. In PDL “Ruffinilike” mechanoreceptor and nociceptive nerve fibers are present, which function to identify and transmit tactile stimulus as well as stimulus to stretching of the PLD fibers.
The stimulus threshold of mechanoreceptors is lower as compared to pain-sensing nociceptive nerve endings. These two separate afferent systems are involved in providing us the information regarding the tooth movement, tooth contact during swallowing, chewing and the jaw position and pain under high occlusal load. This innervation system makes teeth sensitive to identify even a hair between the occluding tooth surfaces. The autonomic innervation originates from the superior cervical ganglion and is primarily responsible for the activation of the smooth muscles associated with vasculature within the PDL 310.
Functions of the periodontal ligament
The PDL performs five major functions: formative, nutritive, proprioceptive, supportive and homeostatic function.
Formative function
The development of PDL takes place from the cells of the dental follicle. Studies have shown that the transplanted cells of the dental follicle have the ability to form the PDL, alveolar bone and cementum 311, 312. This property of synthesizing three different tissues is retained in the PDL and it plays a critical role in periodontal repair and regeneration. Autoradiographic studies indicate a high turnover rate of the PDL collagen 182-185, 313, 314.
Nutritive function
The blood vessels in PDL provide nutrition supply to the cells of PDL, cementocytes and presumably the superficial osteocytes of alveolar bone. The blood vessels are also responsible for the removal of catabolites. In trauma from occlusion, the excessive occlusal load results in the occlusion of the blood vessels leading to cell necrosis in the affected part of the PDL.
Proprioceptive function
One important function of PDL is to provide sensory feedback during the masticatory cycle. As already stated, human teeth are capable of detecting very minute particles between the occluding surfaces. The sensory nerve endings in the PDL provide us the information about how hard and fast to bite. In a study, Williams et al. (1985) 315 anesthetized the teeth and TMJs to measure differences in inter-incisor bite force. It was found that there was a significant discrimination of bite forces only when the teeth were anesthetized. These findings suggest that there is a well-established feedback mechanism in the PDL which plays a significant role in the proper mechanical function of the masticatory system by controlling the magnitude and duration of force application.
Supportive function
Teeth are subjected to forces with different magnitude, direction of application and frequency of application during mastication, speech and orthodontic tooth movement. The PDL plays a central role in withstanding these forces and transferring them to the bone. It has been shown that because the forces during mastication are applied in different directions, both compression and tension areas exist in PDL during a regular loading scheme 306. The mechanical strength of PDL is derived from collagen Type I fibers 316. High degree of vascularization attributes to the ……… Content available in the hard copy of the website……… Content available in the hard copy of the website……………… Content available in the hard copy of the website……… Content available in the hard copy of the website……… Content available in the hard copy of the website………..
Periobasics A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Homeostatic function
The cells of the PDL perform an important task of maintaining normal PDL space and neighboring structures. These cells are capable of resorbing and synthesizing the extracellular substance of PDL, cementum, and alveolar bone connective tissue. It must be remembered that these processes are continuous throughout life with varying intensity. The cells from PDL maintain the normal PDL space by directly influencing the bone deposition or bone resorption of the alveolar bone. This observation is supported by the finding that if a portion or the whole of PDL is irreversibly destroyed; bone deposition takes place in the PDL space, resulting in ankylosis. Another finding associated with PDL homeostasis is the change in PDL space in hypo- and hyper-function. In teeth with hypofunction, the extracellular substance of PDL is lost, resulting in decreased PDL space. Conversely, during hyperfunction the PDL space is increased, presumably to compensate for the increased load.
Know More…
The behavior of the periodontal ligament under forces:
As already stated, PDL plays an important role in transferring the occlusal forces from tooth to alveolar bone. Two theories have been explained for the mechanism of tooth support by periodontal ligament under occlusal forces,
Tensional theory:
According to this theory, the principal fibers play a major role in supporting the tooth and transmitting the forces to the bone. On applying the load, principal fibers unfold and straighten to transmit the forces to alveolar bone, causing elastic deformation of the socket.
Viscoelastic theory:
This theory emphasizes the primary role of fluid movement during tooth movement in the socket with fibers playing only a secondary role. On applying load on the tooth, the extracellular fluid is pushed from periodontal ligament into marrow spaces through the cribriform plate. When the load is removed, this fluid again returns back to PDL space and the normal fluid equilibrium is achieved.
Remodeling of the periodontal ligament
A well-coordinated synchronized action of multiple cell types and signaling pathways is involved in the remodeling of PDL. The term remodeling and turnover should be differentiated here. Turnover constitutes no change in the structural organization of the tissue while remodeling implies positional or functional changes in the tissue. The remodeling of PDL is an important component of its property of adaptability to changes in the functional load 321. Primary cells involved in PDL remodeling are fibroblasts which are responsible for the formation and remodeling of PDL fibers. During remodeling, collagen mesh that stretches from bone to cementum must be rapidly broken down and synthesized. It has been shown that the remodeling of the ligament in continuously growing molars is restricted to the “intermediate plexus” 322. In contrast, another study on partially erupted teeth has reported PDL remodeling throughout the PDL from the cementum to bone 323.
It must be remembered that the remodeling of the PDL fibers takes place in such a way that there is only regional breakdown of the collagen meshwork without compromising the integrity of the tissue on the whole 229, 316. During this process, the collagen breakdown is controlled intracellularly through phagocytosis 229. The precise removal of the collagen fibers is controlled by an intracellular mechanism along with an extracellular collagenase activity. Under long-term loading, there is altered collagen synthesis, promotion of collagenase activity, stimulation of cell division and release of transforming growth factor-β in PDL 324-328. These findings suggest that the PDL may be involved directly or indirectly in bone remodeling also. The fibroblasts and osteoblasts present in the PDL have the required signaling and effector mechanisms to sense and respond to the external load via remodeling 229.
Conclusion
The periodontal ligament plays a very vital role in the maintenance of the various components of the periodontium. It is a highly dynamic tissue, rich in cellular components. Various cells present in the periodontal ligament actively participate in the remodeling of the periodontal ligament, cementum, and alveolar bone. Periodontal ligament plays a vital role in periodontal regeneration. It has been demonstrated by various studies that new attachment involves the formation of alveolar bone, periodontal ligament, and new cementum. Thus, in-depth knowledge of the structure and function of periodontal ligament is essential to understand periodontal regeneration.
References
References are available in the hard copy of the website
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Suggested reading

